Read about the advantages of intraoperative ultrasound in the detection of liver tumours and the planning of surgery.
Mathieu D'Hondt, MD
Dept. of Digestive and Hepatobiliary and Pancreatic Surgery, AZ Groeninge Hospital, Kortrijk, Belgium

Liver resection is the standard treatment for colorectal liver metastases and has a five-year overall survival rate estimated to be as high as 58%1. However, up to 75% of patients undergoing liver resection for colorectal liver metastases will develop intrahepatic recurrence2. The modern treatment of colorectal liver metastases is based on a multidisclipinary approach. From a surgical point of view, the management of colorectal liver metastases has significantly changed over recent years.
Initially contraindicated for surgery, bilateral, synchronous, and recurrent lesions are now eligible for surgery due to the evolution of chemotherapy and patient management options. Historically, parenchymal sparing approaches were considered less effective, due to the theoretical impossibility of achieving satisfying resection margins. Based on the fact that a 1 mm margin is sufficient to be considered curative, and that more extended margins do not lead to oncological benefits in terms of recurrence, more and more parenchyma-preserving liver resections are currently being performed for colorectal liver metastases.
Recently, two large studies of more than 400 patients undergoing hepatic resection for colorectal liver metastases have been published3,4. In both studies, more than 50 patients underwent a repeat hepatectomy, and the studies have shown that a repeat hepatectomy for a single recurrent colorectal liver metastasis is as effective as the first liver resection. Furthermore, one of these studies has shown that the performance of a repeat hepatectomy was independently associated with increased overall and cancer-specific survival following index hepatectomy.
Case presentation:
The patient is a 67-year-old man who had an anterior resection for an adenocarcinoma of the sigmoid in 2003. He developed a solitary colorectal liver metastasis in segment 6 in 2006, and a laparoscopic resection of segment 6 was performed. Two years later, he developed a new solitary colorectal liver metastasis in segment 7. A repeat laparoscopic metastasectomy in segment 7 was performed.
In 2012, the patient developed another colorectal liver metastasis in the left lateral sector. A laparoscopic left lateral sectionectomy was performed, and the patient received 12 cycles of chemotherapy. Until March 2016, there was no evidence of disease.
In 2015, the patient underwent repair of a large ventral hernia with placement of a prosthesis. In February 2017, imaging of the liver showed the presence of a large colorectal liver metastasis in segment 4A of the liver. Based on preoperative imaging, the liver metastasis seemed in contact with the middle hepatic vein. In March 2017, intraoperative ultrasound showed that the large central colorectal liver metastases had grown into one of the branches of the middle hepatic vein. The lesion also effaced the main branch of the middle hepatic vein, so a segment 4A resection was performed with en block resection of the middle hepatic vein. We performed an open liver resection due to extensive adhesion formation.
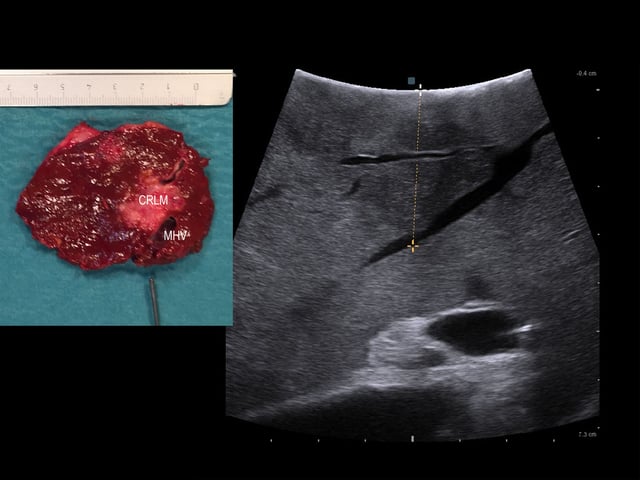 Intraoperative ultrasound: colorectal liver metastasis (CRLM) has grown into one of the branches of the middle hepatic vein (MHV).
Intraoperative ultrasound: colorectal liver metastasis (CRLM) has grown into one of the branches of the middle hepatic vein (MHV).
The lesion has also effaced the main branch of the middle hepatic vein. The resected specimen is shown on the left.
Operative time was 180 minutes, blood loss was 100 cc., and the Pringle manoeuvre was performed for 29 minutes. Parenchymal transection was performed using a bipolar sealing device in combination with a Cavitron Ultrasonic Surgical Aspirator, and central venous pressure during the operation was 3 mm of mercury. The post-operative course was uneventful, and the patient was discharged on day 5 post-operatively. The definitive pathology report confirmed the presence of a 4.5 cm colorectal liver metastases. The resection margins were tumour-free (1.5 cm).
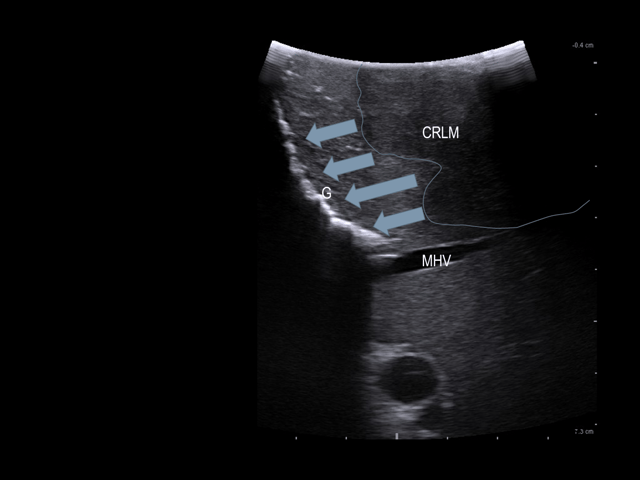 A gauze (G) is placed in the deepest part of the cutting plane. Arrows: tumor-free margin.
A gauze (G) is placed in the deepest part of the cutting plane. Arrows: tumor-free margin.
 Intraoperative view after liver resection
Intraoperative view after liver resection
This case-study was performed under approval by the institutional review board and patient consent, and includes only de-identified patient images. The IOUS was performed with a 10-4.3 MHz T-shaped intraoperative transducer and a BK Ultrasound (Peabody, MA) unit.
Conclusion:
Despite improvements in preoperative imaging, intraoperative ultrasound remains a valuable tool during the resection of colorectal liver metastases. Compared with cross-sectional pre-operative imaging, intraoperative ultrasound is still superior in the detection of liver tumours and the planning of surgery5:
- Intraoperative ultrasound can have an impact on the accurate assessment of the proximity to, or invasion of, the hepatic vasculature which can also influence the operative strategy.
- Intraoperative ultrasound helps the hepatobiliary surgeon to understand the three-dimensional relationship between the liver vasculature and tumour.
- It also improves patient outcome by defining adequate margins of resection and by selecting the correct type of resection.
- The use of intraoperative ultrasound may lead to a change in the operative plan and occasionally allows a less extensive parenchymal preserving resection to be performed6.
Click here to read more about BK Ultrasound's solution for intraoperative surgery.
1 Haddad Aj, Bani Hani M, Pawlik TM et al. Colorectal liver metastases. Int J Surg Oncol 2011; 2011: 285840. doi: 10.1155/2011/285840
2 Simmonds PC, Pimrose JN, Colquitt JE et al. Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer. 2006 Apr 10;94(7):982-99
3 Lee H, Choi SH, Cho YB et al. Repeat hepatic resection in patients with colorectal liver metastases. World J Gastroenterol. 2015;21(7):2124-30.
4 Neal CP, Nana GR, Jones M et al. Repeat hepatectomy is independently associated with favorable long-term outcome in patients with colorectal liver metastases.Cancer Med. 2017 Feb;6(2):331-338
5 D’Hondt M, Vandenbroucke-Menu F, Préville-Ratelle S et al. Is intra-operative ultrasound still useful for the detection of a hepatic tumour in the era of modern pre-operative imaging? HPB (Oxford). 2011 Sep;13: 665-9.
6 Knowles SA, Bertens KA, Croome KP et al. The current role of intraoperative ultrasound during the resection of colorectal liver metastases: A retrospective cohort study. Int J Surg. 2015;20:101-6.
